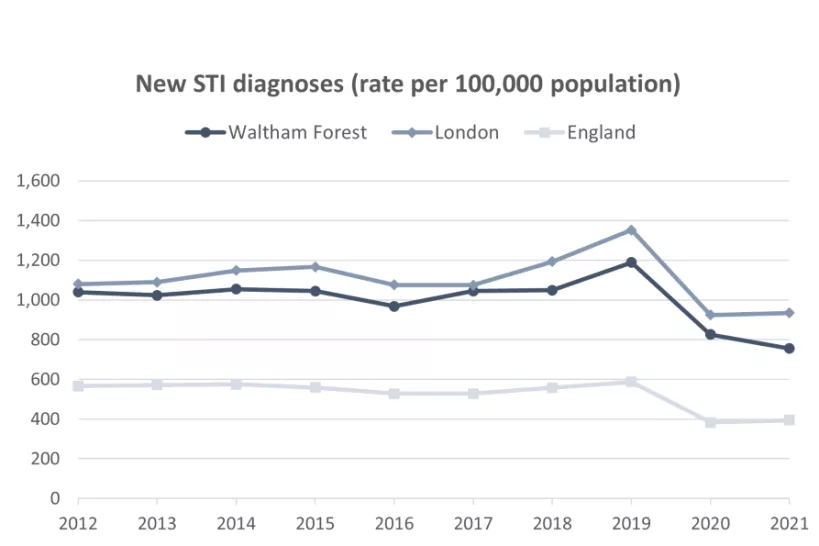
Definition: A summary figure of all new STI diagnoses, excluding diagnoses of chlamydia in the age group under 25, among people accessing sexual health services.
Source: OHID Public Health Outcomes Framework. Data from UK Health Security Agency (UKHSA). Date accessed: 25 April 2023.
To get a fuller understanding of STI prevalence, diagnosis rates should be interpreted alongside data on STI testing and positivity rates. While a high diagnosis rate may be indicative of a high level of infection, a low diagnosis rate may be explained by factors beyond low levels of infection, such as a low testing rate.
In Waltham Forest, the STI testing rate is below the London average and has not yet recovered to pre-pandemic levels. However, the STI testing positivity (the proportion of people testing positive) is also lower the London average (7.2% and 7.9% respectively) as is the rate of new STIs detected. [3]
While the new STI diagnoses indicator considers a range of infections combined, there have been different trends in rates of diagnosis of individual infections; for example, the rate of preventable bacterial sexually transmitted infections such as chlamydia and gonorrhoea in England has been increasing up to 2019, whereas the rate of genital warts has been declining following the introduction of the HPV vaccination programme in September 2008. [4]
References:
[1] Public Health England (2019). Health matters: preventing STIs. Date accessed: 09 June 2023
[2] WHO (2017). Antibiotic-resistant gonorrhoea on the rise, new drugs needed. Date accessed: 09 June 2023
[3] Public Health England (2021). Health Profile for England 2021. Date accessed: 04 May 2023.
[4] Office for Health Improvement & Disparities. Sexual and Reproductive Health Profiles. Data from UK Health Security Agency (UKHSA). Date accessed: 25 April 2023.