Last updated: 15 August 2023
Next review: 20 June 2024
This content is part of the Waltham Forest JSNA. To see other JSNA content, visit the JSNA landing page
Sexually transmitted infections (STIs) are a major public health concern. STIs are often considered to be stigmatising and may seriously impact the health and wellbeing of affected individuals, as well as being costly to healthcare services. If left undiagnosed and untreated, common STIs may cause complications and long-term health problems, including pelvic inflammatory disease, infertility and adverse pregnancy outcomes. Some STIs can also be transmitted from mother-to-child during pregnancy and childbirth. [1]
There is a growing global problem of antimicrobial resistance amongst bacterial STIs, especially for gonorrhoea. This means that antibiotics that are normally used to treat certain STIs are no longer effective, making some cases much more difficult, or even impossible to treat.
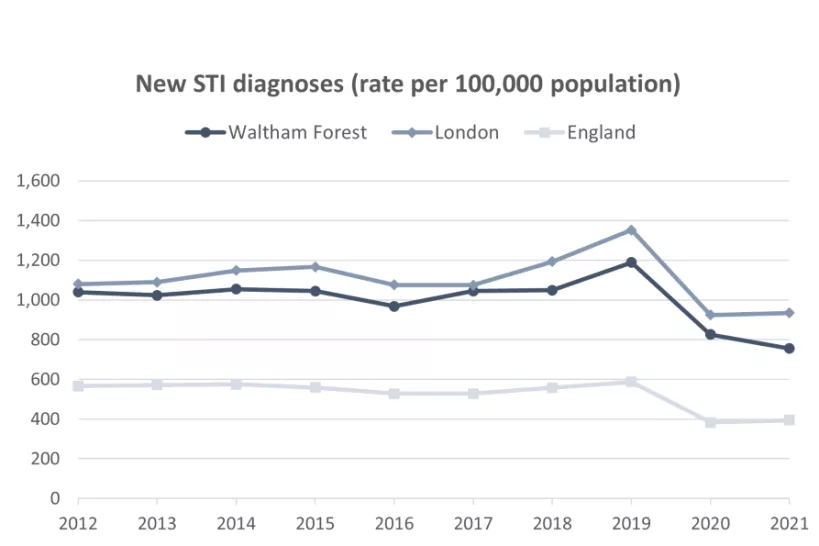
In 2020, the detection rates of STIs declined across the country because of the reduced access to the sexual health services during the pandemic. The reduced demand for sexual health services were likely impacted by the social distancing measures but may also indicate changes in individual risk perception and behaviour and a greater burden of undetected infections in the community. [1]
The rate of new STI diagnoses (including HIV, syphilis, gonorrhoea and chlamydia) in London has consistently been considerably higher than the England average (935 per 100,000 compared to 394 per 100,000 respectively in 2021). Waltham Forest has a lower diagnosis rate than London: 756 new STI diagnoses per 100,000 population as of 2021. There is a significant variation in STI diagnosis rates across London, from 2,634 per 100,000 in Lambeth to 297 per 100,000 in Sutton in 2021.
Definition: A summary figure of all new STI diagnoses, excluding diagnoses of chlamydia in the age group under 25, among people accessing sexual health services.
Source: OHID Public Health Outcomes Framework. Data from UK Health Security Agency (UKHSA). Date accessed: 25 April 2023.
To get a fuller understanding of STI prevalence, diagnosis rates should be interpreted alongside data on STI testing and positivity rates. While a high diagnosis rate may be indicative of a high level of infection, a low diagnosis rate may be explained by factors beyond low levels of infection, such as a low testing rate.
In Waltham Forest, the STI testing rate is below the London average and has not yet recovered to pre-pandemic levels. However, the STI testing positivity (the proportion of people testing positive) is also lower the London average (7.2% and 7.9% respectively) as is the rate of new STIs detected. [3]
While the new STI diagnoses indicator considers a range of infections combined, there have been different trends in rates of diagnosis of individual infections; for example, the rate of preventable bacterial sexually transmitted infections such as chlamydia and gonorrhoea in England has been increasing up to 2019, whereas the rate of genital warts has been declining following the introduction of the HPV vaccination programme in September 2008. [4]
References:
[1] Public Health England (2019). Health matters: preventing STIs. Date accessed: 09 June 2023
[2] WHO (2017). Antibiotic-resistant gonorrhoea on the rise, new drugs needed. Date accessed: 09 June 2023
[3] Public Health England (2021). Health Profile for England 2021. Date accessed: 04 May 2023.
[4] Office for Health Improvement & Disparities. Sexual and Reproductive Health Profiles. Data from UK Health Security Agency (UKHSA). Date accessed: 25 April 2023.